Reflux After Sleeve Gastrectomy
Understanding Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid frequently flows back into the esophagus, leading to uncomfortable symptoms like heartburn, regurgitation, and difficulty swallowing. Acid Reflux after bariatric surgery is a condition particularly common among bariatric patients, with up to 30% experiencing GERD symptoms. The root cause of GERD involves a weakened lower esophageal sphincter (LES), which normally acts as a barrier to prevent stomach contents from moving backward. When the LES is compromised, combined with increased intra-abdominal pressure and impaired esophageal clearance, it results in the backflow of acid into the esophagus. Understanding these mechanisms is crucial for developing effective treatment strategies and improving patient outcomes.
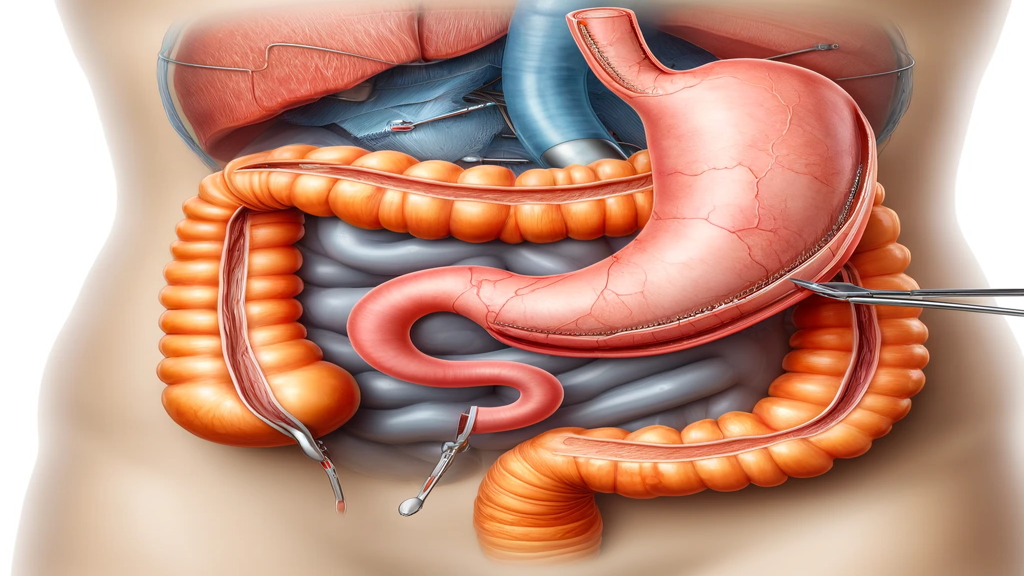
Reflux After Sleeve Gastrectomy
Heartburn is an uncomfortable sensation or pain in your chest, just behind the sternum or breastbone. It is caused by the acid secreted in the stomach traveling up into the esophagus (acid reflux). If the symptoms of acid reflux occur more than twice a week, you might have a condition called gastroesophageal reflux disease (GERD). Acid reflux after sleeve gastrectomy is a frequently discussed topic among bariatric surgeons.
Many studies have shown that approximately 30% of gastric sleeve patients may experience new reflux among those who never had acid reflux before surgery. On the other hand, among the patients who have mild to moderate symptoms of reflux before sleeve gastrectomy, most feel symptomatic relief after surgery because weight loss can decrease the intra-abdominal pressure. However, a subset of patients with reflux prior to surgery may experience worsening of acid reflux post-operation.
What is the cause of reflux after sleeve gastrectomy?
After sleeve gastrectomy, the stomach is significantly smaller and can only hold 100-300 ml of food or liquids at one time. Therefore, the pressure within the smaller stomach is significantly higher. The Lower Esophageal Sphincter (LES) usually prevents the stomach content from traveling into the esophagus. However, with much higher pressure after sleeve gastrectomy, some gastric content or gastric acid gets pushed into the esophagus, causing reflux.
Changes in the gastroesophageal pressure gradient also contribute to reflux after sleeve gastrectomy, as the altered pressure dynamics can lead to increased esophageal reflux and related complications.
Hiatal Hernia and GERD After LSG
A hiatal hernia is a condition where part of the stomach pushes up through the diaphragm into the chest cavity, which can significantly contribute to the development of GERD after laparoscopic sleeve gastrectomy (LSG). This anatomical change allows stomach acid to more easily flow back into the esophagus, exacerbating GERD symptoms. Research indicates that LSG can worsen a pre-existing hiatal hernia, leading to increased acid reflux. To mitigate these issues, concomitant hiatal hernia repair during LSG may be necessary. This combined approach can help alleviate GERD symptoms and prevent long-term complications, ensuring a better quality of life for patients.
Treatment Options for Acid Reflux After Sleeve Gastrectomy
For sleeve gastrectomy patients with mild to moderate reflux symptoms who have regained a significant amount of weight, conversion to Roux-en-Y gastric bypass surgery, a common bariatric procedure, may lead to both weight loss and resolution of reflux symptoms. For those who had difficulty eating due to severe reflux, the weight loss after conversion to Roux-en-Y gastric bypass surgery might be very limited. However, most patients report dramatically improved quality of life because they no longer suffer from heartburn.
Symptoms of Reflux After Gastric Sleeve Surgery
Symptoms of reflux after gastric sleeve surgery can vary in severity and frequency. Common symptoms include:
Heartburn: A burning sensation in the chest and throat, often worsening after eating or when lying down.
Regurgitation: The sensation of food or stomach acid flowing back up into the mouth, causing an unpleasant taste.
Difficulty swallowing: Trouble swallowing food or feeling like food is stuck in the throat, which can be uncomfortable and alarming.
Chest pain: Pain or discomfort in the chest or upper abdomen, which can sometimes be mistaken for heart-related issues.
Bloating and gas: Feeling uncomfortably full or bloated, often accompanied by excessive gas.
Nausea and vomiting: Feeling queasy or vomiting after eating, which can significantly impact your ability to enjoy meals.
These symptoms are caused by stomach acid flowing back up into the esophagus, irritating its lining and causing discomfort. In some cases, symptoms can be severe and interfere with daily activities, making it crucial to seek medical advice if you experience any of these issues after gastric sleeve surgery.
Diagnosis of Reflux After Bariatric Surgery
Diagnosing reflux after gastric sleeve surgery typically involves a combination of medical history, physical examination, and diagnostic tests. Your doctor may:
Review your medical history: Understanding your symptoms and any previous treatments helps in forming a comprehensive picture of your condition.
Perform a physical examination: Checking for signs of reflux, such as inflammation or scarring in the esophagus, can provide immediate clues.
Order diagnostic tests: Tests such as endoscopy, upper GI series, or pH monitoring are often used to confirm the diagnosis and assess the severity of reflux.
Endoscopy involves inserting a flexible tube with a camera and light on the end into the mouth and guiding it through the esophagus and stomach. This allows the doctor to visualize the esophagus and stomach lining and check for signs of inflammation or scarring.
Upper GI series involves swallowing a liquid that contains barium, which helps to visualize the esophagus and stomach on X-ray images.
pH monitoring involves inserting a small tube through the nose and into the esophagus to measure the acidity of the esophagus over a 24-hour period.
These diagnostic tools help in accurately identifying the presence and severity of reflux, ensuring that you receive the most appropriate treatment.
Postoperative Care for Reflux After Bariatric Surgery
Postoperative care for reflux after gastric sleeve surgery typically involves a combination of lifestyle changes, dietary modifications, and medical treatment. Your doctor may recommend:
Lifestyle changes: Losing weight, quitting smoking, and avoiding tight clothing can significantly reduce reflux symptoms.
Dietary modifications: Eating smaller, more frequent meals, avoiding trigger foods, and not lying down immediately after eating can help manage symptoms.
Medical treatment: Medications such as antacids, histamine-2 (H2) blockers, or proton pump inhibitors (PPIs) can reduce acid production and alleviate symptoms.
In some cases, your doctor may recommend further treatment, such as:
Gastric bypass surgery: This procedure can reduce acid production and alleviate symptoms, especially in patients with severe reflux.
Hiatal hernia repair: If a hiatal hernia is contributing to reflux symptoms, repairing it can provide significant relief.
Endoscopic treatments: Procedures like radiofrequency ablation or transoral incisionless fundoplication (TIF) can strengthen the lower esophageal sphincter and reduce reflux symptoms.
It’s essential to follow your doctor’s recommendations and attend follow-up appointments to monitor your symptoms and adjust your treatment plan as needed. By adhering to these guidelines, you can manage reflux symptoms effectively and improve your quality of life after gastric sleeve surgery.
Managing Acid Reflux After Bariatric Surgery
Effectively managing acid reflux after bariatric surgery involves a multifaceted approach that includes lifestyle modifications, dietary changes, and medical treatments. Patients are advised to avoid trigger foods such as fatty, spicy, and acidic items, and to adopt a more restrictive diet to minimize symptoms. Other helpful strategies include quitting smoking, avoiding tight-fitting clothing, and not eating right before lying down. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production, but long-term use can lead to dependency and other side effects. For those with recalcitrant gastroesophageal reflux disease, alternative treatments like laparoscopic magnetic sphincter augmentation may be necessary to provide relief.
Biliary Reflux After Bariatric Surgery
Biliary reflux, a common complication after bariatric surgery, particularly gastric bypass surgery, occurs when bile flows back into the stomach and esophagus. This can cause symptoms such as heartburn, regurgitation, and abdominal pain. The pathophysiology of biliary reflux involves a complex interplay of factors, including gastroduodenal dysmotility, impaired esophageal clearance, and increased intra-abdominal pressure. Treatment options for managing biliary reflux include proton pump inhibitors (PPIs) and antacids to neutralize stomach acid. In more severe cases, surgical interventions such as laparoscopic fundoplication may be necessary to provide relief and improve patient outcomes.
Contact Us
If you have any further questions or concerns about acid reflux after sleeve gastrectomy, please do not hesitate to contact our bariatric clinic. Our experienced team is here to provide you with the information and support you need. Reach out to us today to schedule a consultation and take the first step toward better health and improved quality of life.
FAQS
It’s a follow-up surgery for individuals who’ve had previous bariatric surgery but need modifications due to complications or insufficient weight loss.
Due to weight regain, surgical complications, or not achieving sufficient weight loss from the first surgery.
The procedure varies based on individual needs, ranging from converting to a different type of bariatric surgery to correcting specific complications.
Risks include infection, bleeding, and complications related to anesthesia, similar to those associated with any surgical procedure.
Yes, it can potentially improve outcomes, especially when accompanied by lifestyle changes and medical guidance.
Roux-en-Y gastric bypass (RYGB) surgery is highly effective for morbidly obese patients in achieving substantial weight loss. Studies have shown that RYGB produces significantly greater weight loss compared to lifestyle modifications alone. Additionally, RYGB can alleviate symptoms of gastroesophageal reflux disease (GERD), making it a beneficial option for those suffering from both obesity and GERD.
Proton pump inhibitors (PPIs) are commonly used as a primary treatment for gastroesophageal reflux disease (GERD). They work by reducing gastric acid secretion, which helps in facilitating mucosal healing. However, a significant percentage of patients do not achieve complete symptom relief with PPIs alone. This limitation often necessitates alternative treatments or interventions for those who remain dependent on these medications.
Risks include infection, bleeding, and complications related to anesthesia, similar to those associated with any surgical procedure
Yes, it can potentially improve outcomes, especially when accompanied by lifestyle changes and medical guidance.